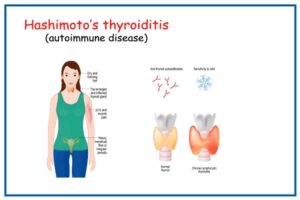
The human microbiome is a complex, interdependent ecosystem. Picture it like a rainforest with lots of different species living in symbiosis. Symbiosis is any type of close and long-term biological interaction between two different biological organisms, and in this case, the organism is your gut microbiome. Your human microbiome has many important jobs, one of which is colonization resistance; it defends against the invasion of pathogenic bacteria. When our immune system and the microbiome are unable to do the job, we turn to antibiotics. Antibiotics are reliable killers of pathogenic bacteria. They kill all of the bacteria along with the bacteria’s family, they also kill all of their friends, their friends of friends, and their acquaintances. Basically, antibiotics kill everything, good or bad. Antibiotics are such reliable killers of pathogenic bacteria that almost all of us have taken them at some point.
Why Antibiotics Are Prescribed
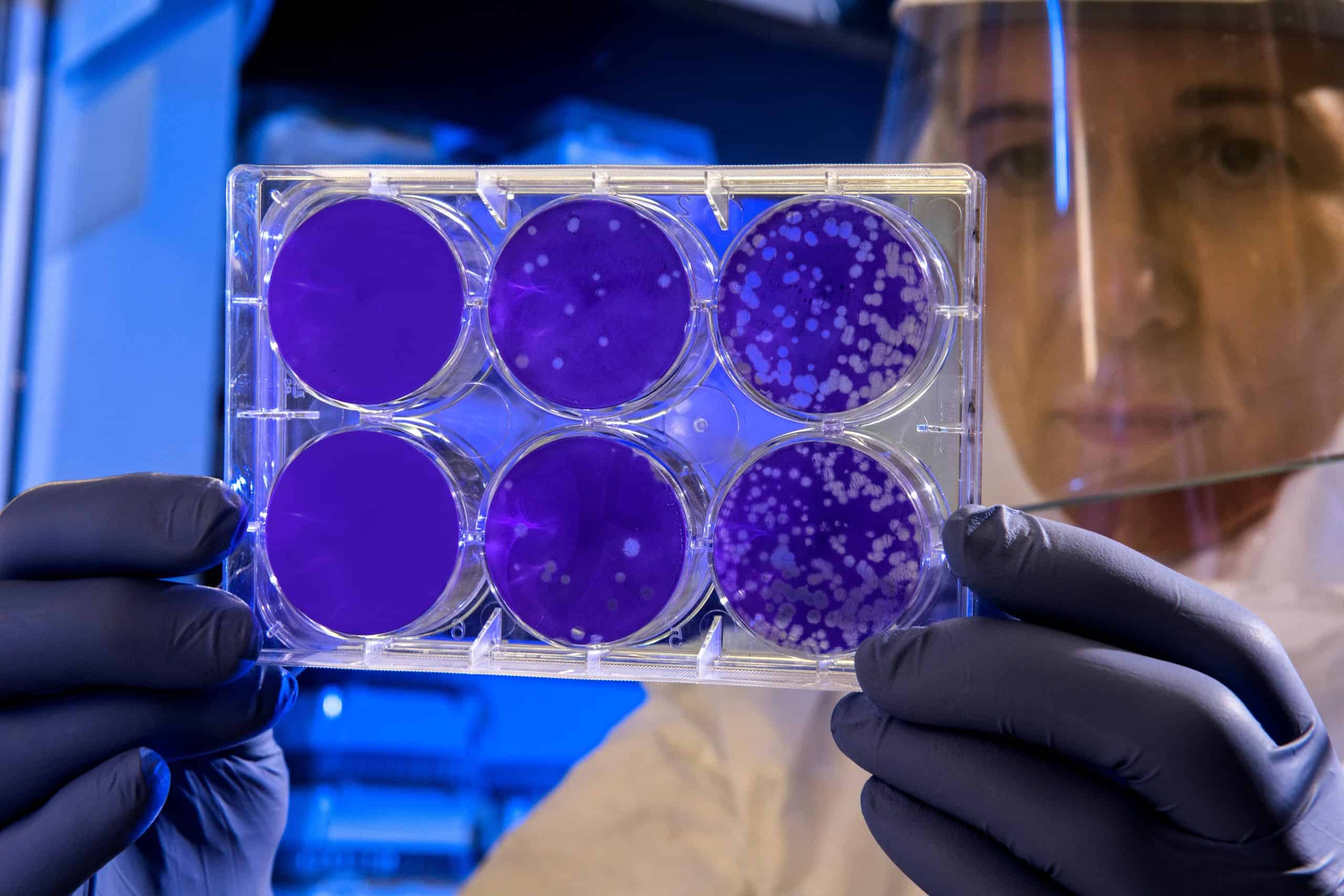
The main reason antibiotics are prescribed is for colds and flu, which is interesting because colds and flu are caused by viruses, not bacteria. Of course, antibiotics are extremely helpful and even life-saving when they are prescribed appropriately. The main side effect you will notice when taking a course of antibiotics is diarrhea – this is due to the sterile effect the antibiotics have on your gut microbiome. Antibiotics can also disrupt the normal function of the human microbiome by reducing diversity and causing dysbiosis. Dysbiosis is a term for a microbial imbalance or maladaptation on or inside the body, such as an impaired microbiota. During a state of dysbiosis is when pathogenic bacteria can strike.
Think of…
- Helicobacter Pylori
- Clostridium Difficile
- Streptococcus
- Staphylococcus
- Blastocystis Hominis
- Giardia
- Etc…
If you’re reading this article, this probably doesn’t apply to you, but it might be helpful if you have children. Antibiotics can be particularly harmful to the microbiome of children. Unfortunately, the lower diversity in a child’s microbiome makes it more difficult to recover from a course of antibiotic use and children generally end up with lower numbers of beneficial bacteria such as lactobacillus and bifidobacteria. In some cases, the profile of the gut microbiome can remain permanently altered.
Another thing one must consider is how intelligent and resilient bacteria are, some bacteria will always survive and become antibiotic-resistant — this means that if you become infected again, the antibiotics will not work to alleviate the infection and you will have to rely on your innate and adaptive immune system i.e. natural immunity.
Helpful Tips
- Only take antibiotics when absolutely necessary. If you are dealing with a skin infection such as cellulitis or staph, try to use topical/local antibiotics first before turning to the oral solution.
- When using oral antibiotics, finish the entire course. This is to ensure that you kill off all of the pathogenic bacteria, including the ones that put up a good fight and try to resist.
- Use Saccyomyces Boulardii during and for 2 weeks after your course of antibiotics. Saccromyces Boulardii is a beneficial yeast that works in a similar way to probiotics except that it is a yeast and not a bacteria, therefore it is antibiotic resistant and will not get killed off during your course.
If you are like me and you have an extensive history of antibiotic use, particularly as a child, it is probably a good idea for you to consult an integrative practitioner who specializes in gut health in order to rebuild the resilience and colonization resistance that your gut once had. If you don’t know where to find such practitioners, reach out to me and the team at Humanli and we will be happy to help you. You can do that by clicking here.
Best,
Marko